“Been in America”: Interviews with German researchers in the USA and Canada

Dr. Hyatt Balke-Want
© Privat
(09/26/22) Through its research fellowship program and Walter Benjamin Fellowship, the DFG supports early-career academics by funding an independent research project abroad and, since 2019, in Germany too. A large proportion of these fellowships are awarded in the USA and Canada, reflecting the belief still prevalent in many disciplines – and in the life sciences in particular – that for a career in research it is helpful to have “been in America.” In a series of interviews, we aim to give you an impression of the wide range of DFG funding recipients. In this edition we take a look at who is behind funding number BA 7065.
DFG: Dr. Balke-Want, thank you so much for taking the time to talk to the DFG’s North American office. Your first name is reminiscent of a US hotel chain and in your CV it says you were born in Srinagar, in the Indian part of the disputed Kashmir Valley between India, Pakistan and China. Let’s start right away with your biography and how you came to Germany – which is probably a much colder place.
Hyatt Balke-Want (HB-W): Thank you very much for this opportunity to speak with you, and of course thank you very much for sponsoring my research stay here on the West Coast. My first name could actually be distantly related to the hotel chain. But in truth my parents wanted to give me a name that signalled their Muslim faith, and Hyatt – Arabic for life – was a good choice. The name is probably more familiar in the female form “Hayet,” but despite its rarity, I still don’t get a discount at the hotel chain. However, I was mistaken for a hotel chain employee by a patient during my nursing internship.
DFG: Tensions between Hindus and Muslims in the Indian part of Kashmir rose to the level of sporadic violence in the late 1980s. When did you move from Kashmir to Germany?
HB-W: My parents emigrated to Germany very soon after I was born. It was helpful that my grandfather ran a small travel agency in Srinagar, an attractive spot with a tradition of tourism, so that meant he had contacts in Germany. An acquaintance helped my father get established in Germany, and it wasn’t long before he had us join him. My father then set up his own business as a goldsmith in Cologne and was able to provide for his wife and two children. I have a brother who is five and a half years younger.
DFG: In addition to the DFG research fellowship, your CV also lists funding from the Hertie Foundation, the Fulbright Commission, the Heinrich Böll Foundation and the German Academic Scholarship Foundation. The funding you received through the Hertie Foundation was from 2006 to 2007, so probably before you left secondary school. How did that come about?
HB-W: I don’t want to offend my scholarship donors and I am very, very grateful for the funding, but I very much fitted the bill in terms of what they define as “worthy of funding”: I have a migrant background, non-academic parents, did well at school and was involved in volunteer work at my handball club. I stumbled upon a Hertie Foundation leaflet at school: I was an avid reader and didn’t want to burden my parents with extracurricular book requests. The Hertie Foundation gave me great support under the START scholarship program.
DFG: During your studies in Witten and at the University of Cologne, you worked on the treatment of lung cancer in your doctoral thesis. Where did this interest come from?
HB-W: Shortly before my studies, I did a nursing internship in oncology at the University Hospital in Cologne and around the same time my grandfather died of bronchial carcinoma in Srinagar – as a non-smoker, it must be said. With lung cancer, a distinction is drawn between small cell tumours (SCLC) and non-small cell tumours (NSCLC). While high-throughput sequencing of the tumour genome can now be used to gain key insights into the latter in terms of therapy, SCLC – which accounts for about 10% of all lung cancer cases and between 7,000 and 8,000 cases per year in Germany – currently still has a five-year survival rate of less than 7%. It’s brutal, and understanding it requires more fundamental molecular biology insights – as well as raising really good scientific questions, as I found out when I did my doctorate with Dr. Roman Thomas.
DFG: You then stayed in Cologne after your doctorate but switched to Dr. Michael Hallek to work clinically in haemato-oncology. Why the change?
HB-W: I just wanted to finally apply what I’d learned in my studies and independently care for people struggling with health problems. I also had this idea that my clinical practice would enable me to discover new inspiring approaches for my scientific work. As things turned out, I actually was very lucky to be able to treat patients with a novel cellular immunotherapy under the guidance of Prof. Hallek and Prof. Borchmann. We call these genetically modified cells chimeric antigen receptors, or chimeras for short: CAR-T cells. Despite the often extensive pre-treatments, we see decent and durable response rates in about one third of patients with non-Hodgkin's lymphoma and B-cell leukemia. This immunotherapeutic approach has revolutionized the treatment of a number of cancers, and when you see a tumour of this kind disappear before your eyes after a few days or weeks, you naturally want to apply this type of approach to other kinds of tumours.

Farewell lunch with our lab. The photograph only shows some of the team members
© Privat
DFG: What is to be said against it?
HB-W: Not all cancers are the same and the currently approved immunotherapeutic drugs cost almost half a million euros per patient. I’m doing research into both problems at Stanford in Crystal Mackall’s group. Here they’re working on optimizing all kinds of CAR-T cell therapies for other tumour types and also on producing the cell therapeutics more efficiently and therefore more cheaply. If we could get a therapy of this kind to the patient for something like 50,000 euros each, we could go some way to ensuring that cancer survival was no longer in conflict with the financing of the health system.
DFG: What makes immunotherapy with CAR-T cells so expensive?
HB-W: In broad terms, this is what happens: they take several hundred million T cells from the patient’s blood, purify them and then manipulate them with a viral vector so that they can then fight the tumour in the patient’s body. You ultimately need a sufficient number of manipulated T cells for this purpose. As a rule, however, the whole process doesn’t happen on site where the patient is treated: the patient’s unpurified blood is first sent to a production center. But for that to happen, the production center has to have a slot free to produce the cells. Only then can the blood be taken from the patient and sent in. After production, the cells are sent back to the treatment site. So an enormous logistical effort is required! And then there is the cost of the viral vector and its testing. The cost of a batch of virus of this type is often in the six-digit range, and the number of patient products that can be produced with one batch is not always precisely predictable. It depends on how concentrated the virus supernatant is, how potent the viruses are and how the supernatant was filled. We’re currently trying to replace the viral vector step with the CRISPR-Cas9 method and integrate the desired DNA sequence into the patients’ T cells without viruses.
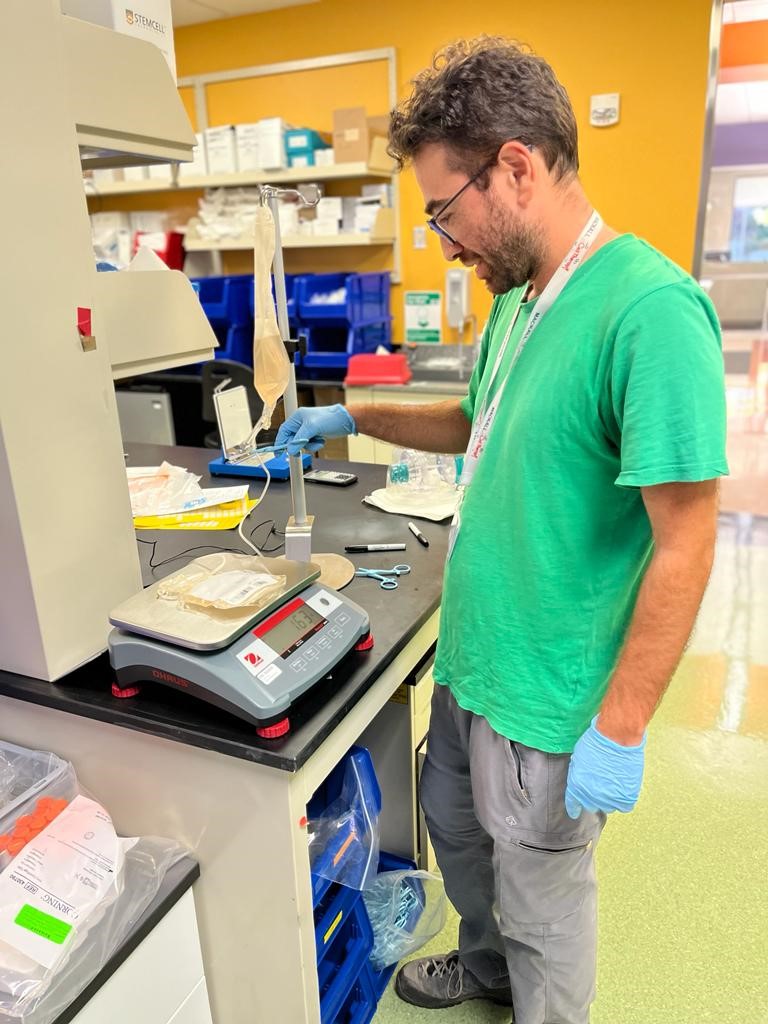
Preparing a scale-up experiment in which we test feasibility for the production of a patient product
© Privat
DFG: Isn’t that also a question of scaling and the relevant production on an industrial scale? Or to put it another way: would a CRISPR-Cas9 process really offer such a cost benefit over the vector process if both were scaled appropriately?
HB-W: That may well be the case. But if you want to clinically test an innovative CAR or other therapeutic transgene on a small group of patients in a university setting, you don’t have a million euros or more available just for the viral vector. That’s an absolute innovation killer. In addition, the CRISPR-Cas9 system allows very specific modifications to be made. Nowadays, everyone talks about precision medicine – in my view, virus transduction with a viral vector is the absolute opposite of this. We can’t control where we insert the desired sequence in the genome: currently we leave this to chance or to the viruses. So not only might we be able to produce these cell therapeutics more cheaply, it might be possible to generate better versions, too.
DFG: What is your typical daily routine like right now? What happened today, for example?
HB-W: I tend to be an early riser so I’m usually up by six o'clock. Our daughter sleeps a little longer, so I have some time for myself to eat my muesli and write e-mails. On a good day I’ll manage to read a paper, too. As soon as our daughter is awake, I very much like to slip into the father role, taking care of her and getting her ready for the day. After that I get on my bike. We live in Redwood City, about ten kilometers from the Stanford University campus. My route takes me through Atherton, past the homes of possibly the richest people on the planet. If I were to take the parallel road, I would pass people who live in caravans because they can’t afford to pay the rents here. Welcome to America.
DFG: Do you feel ambivalent about this?
HB-W: Yes, of course: if you don’t, you’re deliberately shutting your eyes, or you lack empathy or are possibly even cynical. Or you really are blind to the problem – apparently there are people like that, too.
DFG: Then let’s talk about what you really like about your stay at Stanford.
HB-W: I’d love to. There are two main aspects that are probably related. Spending a period of time in North America still seems to be indispensable for an academic career in the life sciences in Germany, and there are probably a number of reasons for this: the groups are more international, more vibrant and at least perceived to be leaner in terms of hierarchy than in Germany; what’s more, there is more money in the system in relative terms, and in absolute terms the system is at least five times as big. Here at Stanford, there is also the fact that the different disciplines work very closely together and the interaction between the development of technologies and the development of research questions pulsates at a high frequency.
DFG: Are the shorter times from bench to bedside – i.e. between understanding and application – in the U.S. due to a better entrepreneurial spirit, or are people simply more reckless?
HB-W: I’m not sure about that, because I’m very inexperienced on the entrepreneurial side.

On an excursion to Yosemite National Park with a view of El Capitan and the Half Dome (with “the commander” in the carrier backpack
© Privat
DFG: You arrived in California for your postdoc in March 2020, coinciding with the first lockdown and the travel restrictions that involved. How did that work out?
HB-W: That almost messed up my entire stay here. I’d already travelled ahead, and my wife and our daughter – who was three months old at the time – were suddenly stuck in Germany. It was something of a drama to re-establish the compatibility of work and family at a single geographical location. Together with the other COVID-19 restrictions, this certainly took six months out of the funding period. But as they say in Cologne: “Et hätt noch jot jejange” (“things have a way of working out somehow”), and thanks to generous COVID-19 arrangements on the part of the DFG and their truly family-friendly funding – many thanks again for this – I was able to carry out my research project with a time delay but essentially as planned, so I will hopefully make my contribution to scientific progress while at the same time being able to fully take on my role as husband and father. My wife is also a doctor and doesn’t want to put her own career plans on hold for good. She is doing so at the moment to support me, but we both agree that this shouldn’t become a permanent state of affairs.
DFG: So your daughter will have a professor as a father?
HB-W: That’s not my primary goal. I can find personal fulfilment and pursue my own ideas through my academic work. What a privilege! Especially if you can improve the care of sick people, too. But you’re right; in order to be able to continue my work in the future, there are a few milestones that have to be reached: publications, finishing my residency and then perhaps doing my postdoctoral teaching qualification – and all that without running my marriage into the ground or neglecting my relationship with my child. Pursuing ambitious professional goals can have a very negative impact on your private life.
DFG: How can this negative impact be kept in check?
HB-W: Communication is the key here. When things are going well, you can and should keep it up, because when things get worse, you need to communicate to stop them getting worse still. As internal medicine specialists, my wife and I sometimes have a difficult role to play in our work because we have to deal with desperate circumstances where the only remedy is to talk to the patient and the relatives. But at the moment I’m doing research “on the bench”; I’m not at the bedside so I don’t have to cope with existential situations of this nature. Day-to-day personal life plays out on a much less dramatic level, but you still shouldn’t neglect communication. We urgently need to teach this to our daughter: my wife and I call her “the commander” because her preferred mode of communication right now is clearly the command expressed as a wish.
DFG: Shall we conclude by taking a look at the crystal ball together? Where will you be in five years’ time with immunotherapy, where will you be in your personal life and what will your daughter take pleasure in when she’s nearly eight years old?
HB-W: As far as our daughter is concerned, that’s easy: she’ll be secretly pleased to find out that even with the best will in the world, you can’t have everything. I will be applying my current work at the bench to the bedside in Germany. And my wife will have long since finished her residency. The picture is not so clear with regard to progress in immunotherapy, or the question of which of the many hopes can actually be justified. It’s an absolutely intriguing field. If I could make a wish, it would be something typically American: “all of the above,” i.e., immunotherapies available for significantly more types of cancer at a reasonable cost, professional self-fulfilment for my wife and myself, and a daughter who is still happy – in other words, the perfect trifecta!
DFG: In that case thank you very much for this entertaining and very informative interview. We wish you well and hope for the very best in the development of immunotherapy, too!